gut brain connection
The gut is now being termed the second brain.
Our ‘gut feelings’ are not just a myth, but a scientific phenomenon.
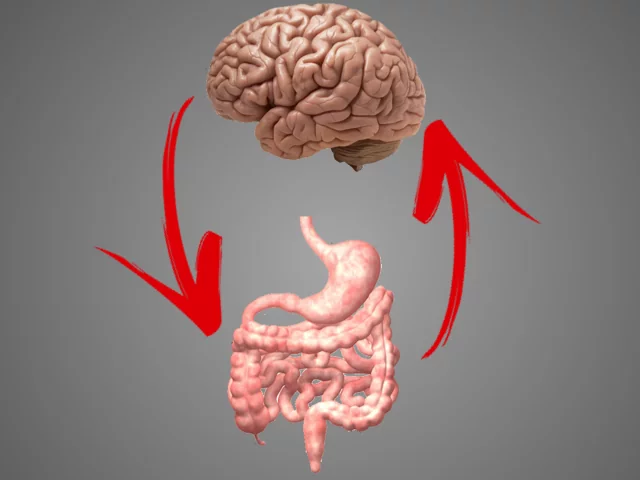
What’s going on in your gut has been shown to affect the health of your brain.
What’s going on in your brain has been shown to also affect the health of your gut.
This two-way communication network between the gut and the brain has been termed the
‘gut-brain axis’.
HOW DOES THIS WORK?
Your gut and brain are connected physically and biochemically through many avenues. Currently, the exact mechanisms of communication between the gut microbiota (all the bacteria that reside in your gastrointestinal tract) and the brain have not yet been defined. However, they do know that your gut microbiota exerts effects on the brain not only through the nervous system but also through the endocrine system, immune system, and metabolic system. [1] The most important communication line between the gut and brain that has been identified is the Vagus Nerve. This runs along your spine. It is the longest nerve in the body beginning at the brainstem, running down the neck, thorax to the abdomen.
DID YOU KNOW?
We are all made up of approximately 10 times more bacteria than we are human cells! Amazing really. How can we possibly ignore the significance of these microbes any longer.
OUR GUT AND MENTAL HEALTH
We are now being flooded with growing evidence that the trillions of microbes that live in our gut (gastrointestinal tract) play a significant role in the health of our brain and our mental health. The colonies of bacteria that reside in your gut influence your behaviour and nervous system; and are capable of producing most of the neurotransmitters also found in the human brain (GABA, Serotonin, Catecholamines, and acetylcholine). [2] [3]
When these neurotransmitters are produced within the gut, they send signals that alter brain function and affect behaviour. Consequently, a serotonin dysfunction in the gastrointestinal system could result in impairments in brain function, such as those involved in mood, sleep, and behaviour[4]. Wow!
The bacteria in our gut can also either decrease or increase inflammation throughout our body and increase the production of cortisol and our stress response[5]. These factors all have a direct influence on our brain.
The wonderful thing is that we now have the technology to test the various species of bacteria that reside within us. We can then use this information to create protocols to assist us in regaining improved microbial balance and greater well-being.
OUR THOUGHTS
We are also learning that the thoughts you have and the stress that you are exposed to, inversely has negative effects on the composition of bacteria that reside in your gut. [6] [7] Stress can increase the growth of bad bacteria and decrease the abundance of good bacteria. This then has a ripple effect, reducing the production of the vital neurotransmitters needed to give you that happy feeling.
Studies have shown that by improving the composition of the microbial colonies in the gut we can see beneficial effects not only on the health of your gut, but also the health of your brain. We can do this through dietary intervention, testing, supplementing (with the correct probiotics and prebiotics), and implementing stress reduction strategies.
Beneficial changes in your gut microbiome can result in better moods and greater quality of life. How good is that!?!

REFERENCES
[1] Hong-Xing Wang1 and Yu-Ping Wang. 2016. Gut Microbiota-brain Axis. Chin Med J (Engl). Oct 5; 129(19): 2373–2380. doi: 10.4103/0366-6999.190667
[2] Dinan TG1, Cryan JF2. 2017. The Microbiome-Gut-Brain Axis in Health and Disease. Gastroenterol Clin North Am. 2017 Mar;46(1):77-89. doi: 10.1016/j.gtc.2016.09.007. Epub 2017 Jan 4.
[3] Wall R, Cryan JF, Ross RP, et al. Bacterial neuroactive compounds produced by psychobiotics. Adv Exp Med Biol. 2014;817:221-39. doi: 10.1007/978-1-4939-0897-4_10.
[4] Miles Berger, John A. Gray, et. al. 2009. The Expanded Biology of Serotonin. Annnual Review of Medicine. Vol. 60:355-366 (Volume publication date February 2009).
[5] Ait-Belgnaoui A, Colom A, Braniste V, et. al. 2014. Probiotic gut effect prevents the chronic psychological stress-induced brain activity abnormality in mice. Neurogastroenterol Motil. 2014 Apr;26(4):510-20. doi: 10.1111/nmo.12295. Epub 2013 Dec 30.
[6] Bailey MT1, Dowd SE, Galley JD, et al. 2011. Exposure to a social stressor alters the structure of the intestinal microbiota: implications for stressor-induced immunomodulation. Brain Behav Immun. 2011 Mar;25(3):397-407. doi: 10.1016/j.bbi.2010.10.023. Epub 2010 Oct 30.
[7] Bailey, M. T., Dowd, S. E., Parry, N. M., Galley, J. D., Schauer, D. B., & Lyte, M. (2010). Stressor Exposure Disrupts Commensal Microbial Populations in the Intestines and Leads to Increased Colonization by Citrobacter rodentium. Infection and Immunity, 78(4), 1509-1519. doi:10.1128/iai.00862-09